This post was originally published on this site
WASHINGTON — Doctors, nurses or pharmacy staff at the Department of Veterans Affairs’ hospitals were fired or reprimanded in only a small fraction of thousands of reported cases of opioid theft and missing prescriptions since 2010, according to government data obtained by The Associated Press.
About 372 VA employees were disciplined for a drug or alcohol-related issue across a network of 160 medical centers and 1,000 clinics over the last six years, according to internal figures kept by the facilities that were reported to VA’s headquarters. During that time, there were more than 11,000 reported incidents of drug loss or theft at federal hospitals — the vast majority within the VA, according to law enforcement data. Roughly translated, VA employees were disciplined in 3 percent of cases.
Nearly one-third of the disciplined employees were dismissed or forced to resign, according to VA data. Others were suspended without pay, admonished or given “last chance” warnings. Disciplined employees had failed a drug test or were suspected of stealing drugs, among other offenses.
The VA declined to comment on reasons behind the low disciplinary rate, saying some cases were still being adjudicated. It also would not immediately release the case reports, citing employees’ personal information.
“We would like there to be no drug diversion anywhere at any time,” Michael Valentino, chief consultant at VA’s Pharmacy Benefits Management Services, told AP. “No matter how robust our systems are, people will be determined to find ways to get around them.”
“It’s a lesson we can learn to tighten things up if possible,” he said.
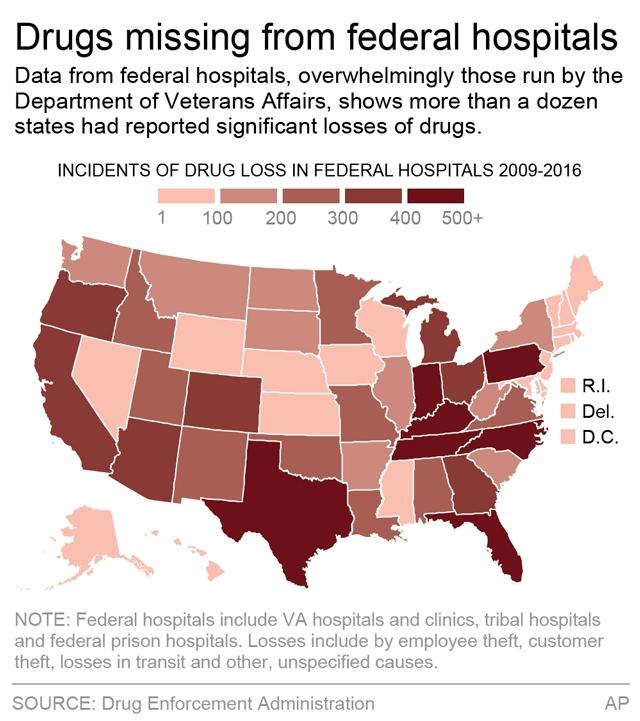
The AP reported last week on government data showing a sharp increase since 2009 in opioid theft and drugs that had simply disappeared at the VA, amid rising opioid abuse in the U.S. Reported incidents of drug losses or theft at federal hospitals jumped from 272 in 2009 to 2,926 in 2015, before dipping to 2,457 last year, according to the Drug Enforcement Administration. “Federal hospitals” include the VA’s facilities as well as seven correctional hospitals and roughly 20 hospitals serving Indian tribes.
Aggravating the problem is that some VA hospitals have been lax in tracking drug supplies. Congressional auditors said spot checks found four VA hospitals skipped monthly inspections of drug stocks or missed other requirements. Investigators said that signals problems for VA’s entire network.
A House panel planned a hearing Monday on the issue. Recent audits also found spotty VA compliance with federal drug testing, for instance failing to test 70 percent — or 15,800 — prospective employees over a 12-month period who would serve in sensitive VA positions such as doctor, nurse or police officer.
“Until VA employees understand that there will be real consequences for misconduct, they’re completely disincentivized from following the rules. We believe that the VA should ramp up drug testing to help weed out those who are abusing the system,” said Dan Caldwell, policy director for the conservative Concerned Veterans for America.
Addressing the Disabled American Veterans group on Sunday, new VA Secretary David Shulkin, who served as the department’s undersecretary of health while the drug problem was growing, listed employee accountability as a top priority. Shulkin said he would work with Congress to pass legislation so that “bad employees are leaving the system.”
The VA said it had strong policies, such as 72-hour inventory checks and “double lock and key access” to drugs, but acknowledged that required inspections and other protocols weren’t being followed consistently.
VA cited its own data showing 2,405 cases of drug loss or theft from January 2014 to March 2016. It said nearly 92 percent of controlled substance losses went missing in transit — describing many as lost in the mail, though acknowledging VA drugs also could have disappeared during employee handling right before mailing. Another 1.5 percent of losses were specifically reported as theft by VA staff, while 1.2 percent was reported as “external theft” and 5.9 percent were attributed to unknown or other reasons such as dispensing errors.
Keith Berge, a Mayo Clinic anesthesiologist who chairs its Medication Diversion Prevention group, said drug theft was serious and patients could be seriously harmed if deprived of medication. Drug addicts are clever and will seek out hospitals where they believe monitoring is weak, he said.
“It is not good enough to merely have effective policies and procedures on the books; they must actually be rigorously followed,” Berge said.
Randall Williamson, health care director at the Government Accountability Office, cited “not a great track record” of accountability at the VA. He said employees who fail to conduct inspections should be held responsible.
“The culture has to be changed,” he said. “The question is whether the VA will quit making excuses and fix the system.”
